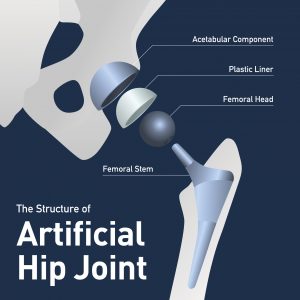
Not all artificial hips fail. Many total hip replacement surgeries are successful. Unfortunately, artificial hips, particularly “metal-on-metal” hips, have “failed” at a rate much higher than previous artificial hip systems, whose components typically consisted of a combination of metals, plastics, and ceramics. The metal-on-metal design placed a metal ball or head directly into a metal acetabular cup. By using a metal cup and a metal ball, these artificial hips forced metal to rub against metal with the full weight and pressure of the human body. As long as the metals held up, all would be well. But it turned out that this intense pressure and movement often caused the metals to grind and deteriorate, and too often releasing metal particles into the surrounding tissue and into the bloodstream. In other artificial hip failures, such as with the Stryker LFIT v40, femoral heads can malfunction due to a failure in the taper lock. The taper lock is the part of the hip prosthesis that connects the femoral head to the stem. This can cause the neck on the femoral stem to grind down (sometimes referred to as “penciling”) and can even lead to a full disassociation (more on that below).
In still other artificial hip failures, the plastic liner (between the cup and ball) deteriorates and causes the total artificial hip system to fail. Polyethylene liners are very important in an artificial hip because over the years, it will serve as a buffer between the metal cup and also the metal femoral head or ball, so it can protect against excessive grinding of the hip components. But the studies have shown that Exactech hip plastic liners have been breaking down and showing signs of premature wear.
Please note that with any hip replacement surgery, there will be a period of rehabilitation. Even with great surgery results, the patient will suffer some soreness, stiffness, and a period to regain strength, mobility, and comfort. From the hundreds of people I have spoken with over the years who have undergone hip replacement surgery, even successful hip replacements do not turn you into a completely pain-free eighteen year old athlete.
 North Carolina Product Liability Lawyer Blog
North Carolina Product Liability Lawyer Blog